Gastric Bypass Surgery For Weight Loss
Gastric bypass procedures (GBP) are any of a group of similar operations that first divides the stomach into a small upper pouch and a much larger lower "remnant" pouch and then re-arranges the small intestine to allow both pouches to stay connected to it. Surgeons have developed several different ways to reconnect the intestine, thus leading to several different GBP names. Any GBP leads to a marked reduction in the functional volume of the stomach, accompanied by an altered physiological and physical response to food.
The operation is prescribed to treat morbid obesity, defined as a BMI greater than 40, and also to treat type 2 diabetes, hypertension, sleep apnea and other co-morbid conditions.Bariatric surgery is the term encompassing all of the surgical treatments for morbid obesity, not just gastric bypasses, which make up only one class of such operations. The resulting weight loss, typically dramatic, markedly reduces comorbidities. The long-term mortality rate of gastric bypass patients has been shown to be reduced by up to 40%; however, complications are common and surgery-related death occurs within one month in 2% of patients.
The most common gastric bypass surgery is a Roux-en-Y gastric bypass.
In normal digestion, food passes through the stomach and enters the small intestine , where most of the nutrients and calories are absorbed. It then passes into the large intestine (colon), and the remaining waste is eventually excreted.
In a Roux-en-Y gastric bypass, the stomach is made smaller by creating a small pouch at the top of the stomach using surgical staples or a plastic band. The smaller stomach is connected directly to the middle portion of the small intestine (jejunum), bypassing the rest of the stomach and the upper portion of the small intestine (duodenum).
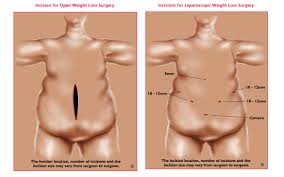
This procedure can be done by making a large incision in the abdomen (an open procedure) or by making a small incision and using small instruments and a camera to guide the surgery (laparoscopic approach).
See a picture of a Roux-en-Y gastric bypass
After surgery, you'll need to make big, permanent changes in how you eat:
Your doctor may only consider doing gastric bypass surgery if you have not been able to lose weight with other treatments.
The following conditions may also be required or are at least considered:
The laparoscopic approach showed similar results, with 69% to 82% of excess weight lost over 12 to 54 months.
Fewer than 10 out of 1000 people die after weight-loss surgery.
After a Roux-en-Y gastric bypass:
In a gastric bypass, the part of the intestine where many minerals and vitamins are most easily absorbed is bypassed. Because of this, you may have a deficiency in iron, calcium, magnesium, or vitamins. This can lead to long-term problems, such as osteoporosis. To prevent vitamin and mineral deficiencies, you may need to work with a dietitian to plan meals, and you may need to take extra vitamin B12 as pills, shots, or nasal spray.
There is also a possibility that you may develop gallstones after gastric bypass. Sometimes the gallbladder is removed as part of the surgery. But if your gallbladder is not removed, then you may need to take medicine to prevent gallstones.
Early studies of the laparoscopic approach to surgery for obesity suggest that it reduces recovery time and postsurgery complications
The physicians in the Michael E. DeBakey Department of Surgery perform the gastric bypass laparoscopically. Using this minimally invasive approach, patients heal faster and are able to return to their normal activities more quickly. They also have much less pain, infections, hernias, and overall complications.
Laparoscopic surgery involves making a series of small incisions and inserting long tube-like instruments through them. The abdomen will be filled with gas to help the surgeon view the abdominal cavity. A camera will be inserted through one of the tubes that will display images on a monitor in the operating room. In this manner, your surgeon will be able to work inside your abdomen without making a larger incision.
Specialized instruments are used to laparoscopically perform the Roux-en-Y Gastric Bypass. This is the same gastric bypass as has been performed with the traditional open approach (large incision), but with superior results.
Step 2: Obtain referral from your Primary Care Physician (PCP) prior to attending our patient information session. In order to attend the information session we will need you to obtain a clearance letter from your PCP. At this time you should also contact your insurance company to verify that weight loss surgery is covered. If they say that they do NOT cover it, please inquire whether they have any exceptions to that policy. Often if you have certain medical conditions they will cover the surgery.
Step 3: Attend patient information session. The next step is to attend one of our free patient information sessions to assist you in determining whether weight loss surgery is for you. You are encouraged to bring a support person to this session. These sessions include detailed overviews of teh surgery, preparation for surgery and postoperative follow up. You will hear from the surgeon, psychologist, nutritionist, nurse practitioner, financial specialist, and our bariatric coordinator to ensure that all your questions and concerns are addressed. The psychologist will inform you of support groups, emotinal eating classes and other strategies for success. Our nutritionist will explain all the nutritional changes to expect and answer any questions you may have about diet, eating post-surgery, etc. This will be the same nutrionist you meet with for your nutrition consult later in the process. We then have a patient financial services representative take you through the financial process and an insurance specialist to advise you on how to get the surgery covered by your insurance company. Finally, you will meet former patients who have had the surgery and hear their stories and ask them any questions you may have about life after bariatric surgery.
Step 4: Begin preauthorization process with insurance company. There are many types of health insurance policies and many have very strict guidelines for reimbursment. Contact your insurance company for verification of coverage and review your particular policy's guidelines and referral requirements, as well as co-payments. During this step you will work closely with the physician's office to assist you with meeting your insurance company's requirements, including documentation to get your surgery approved by your insurance company. Generally documentation about past weight loss attempts are required. Obtaining this information may require some persistance. Persevere - it will be worth the time and effort.
Step 5: Meet with surgeon and set surgery date. This is fairly straightforward - you meet one-on-one with the surgeon to asses where you are in the process and further discuss the details about the surgery. This is an opportunity for you to delve into the details of your personal case and ask any questions you may still have.
Step 6: Preparation for surgery. Once a surgery date has been decided, our team members will work with you to set up your necessary appointments. Everyone will need to have a chest x-ray, blood work, nutrition consult, and psychological consult. Certain patients will also require a gastroscopy (EGD) or upper GI (UGI). During your meeting with the surgeon, we will also decide if additional medical clearance is necessary from a cardiologist, pulminologist or other medical specialist.
Step 7: Day of Surgery. Prior to surgery we will step you through all detailed pre- and post-surgery instructions. The day of surgery you will come to the hospital early with an empty stomach and let our skilled clinical team prepare and care for you!!
Step 8: Begin the process of healing and feeling better. Successful bariatric surgery begins in the operating room, but it ends in the details of your daily life. It is important to be prepared physically and mentally for the life changes you are about to experience. After surgery, staying hydrated is essential. Careful attention to nutrition and keeping a close relationship with your nutritionist is essential. It is easy to become nutrient deficient if you do not comply with post operative vitamin supplementation. Exercise is another vital component to your success. Simple walks and controlled exercise are important as your body begins to loose weight. Remember our team of exercise specialists are happy to help you create the right exercise plan for you.
Many insurance companies will pay for this surgery. Some will require extensive paperwork in order to do so and some will require you to meet certain criteria. The best place to start finding out your insurance plan coverage is to call them and ask if they cover bariatric surgery. If they say no, ask them if there are any exceptions to that policy. Every company has an exclusion section that explains what the company will or will not pay for. In our patient information section we have a document about how to make an appeal to your insurance company as well as a sample letter.




















The operation is prescribed to treat morbid obesity, defined as a BMI greater than 40, and also to treat type 2 diabetes, hypertension, sleep apnea and other co-morbid conditions.Bariatric surgery is the term encompassing all of the surgical treatments for morbid obesity, not just gastric bypasses, which make up only one class of such operations. The resulting weight loss, typically dramatic, markedly reduces comorbidities. The long-term mortality rate of gastric bypass patients has been shown to be reduced by up to 40%; however, complications are common and surgery-related death occurs within one month in 2% of patients.
Gastric bypass
Gastric bypass surgery makes the stomach smaller and allows food to bypass part of the small intestine. You will feel full more quickly than when your stomach was its original size, which reduces the amount of food you eat and thus the calories consumed. Bypassing part of the intestine also results in fewer calories being absorbed. This leads to weight loss.The most common gastric bypass surgery is a Roux-en-Y gastric bypass.
In normal digestion, food passes through the stomach and enters the small intestine , where most of the nutrients and calories are absorbed. It then passes into the large intestine (colon), and the remaining waste is eventually excreted.
In a Roux-en-Y gastric bypass, the stomach is made smaller by creating a small pouch at the top of the stomach using surgical staples or a plastic band. The smaller stomach is connected directly to the middle portion of the small intestine (jejunum), bypassing the rest of the stomach and the upper portion of the small intestine (duodenum).
This procedure can be done by making a large incision in the abdomen (an open procedure) or by making a small incision and using small instruments and a camera to guide the surgery (laparoscopic approach).
See a picture of a Roux-en-Y gastric bypass
What To Expect After Surgery
Most people can return to their normal activities in 3 to 5 weeks.After surgery, you'll need to make big, permanent changes in how you eat:
- You can eat only a few ounces of food at a time. Your new stomach will only hold a tiny amount of food.
- You must eat very slowly and chew your food to mush. Otherwise, you may vomit often and have pain.
- You won't be able to drink for 30 minutes before you eat, during your meal, and for 30 minutes after you eat. There won't be room in your stomach for both drinks and solid food.
- You probably will need to take vitamins and supplements.
- You may have to avoid foods that contain simple sugars-like candy, juices, ice cream, condiments, and soft drinks. Simple sugars may cause a problem called dumping syndrome. This happens because food moves too quickly through the stomach and intestines. It can cause shaking, sweating, dizziness, rapid heart rate, and often severe diarrhea.
Why It Is Done
Although guidelines vary, surgery is generally considered when your body mass index is 40 or higher or you have a life-threatening or disabling condition related to your weight.Your doctor may only consider doing gastric bypass surgery if you have not been able to lose weight with other treatments.
The following conditions may also be required or are at least considered:
- You have been obese for at least 5 years.
- You do not have an ongoing problem with alcohol.
- You do not have untreated depression or another major psychiatric disorder.
- You are between 18 and 65 years of age.
How Well It Works
Most people who have gastric bypass surgery quickly begin to lose weight and continue to lose weight for up to 12 months. One study noted that people lost about one-third of their excess weight (the weight above what is considered healthy) in 1 to 4 years. Some of the lost weight may be regained.The laparoscopic approach showed similar results, with 69% to 82% of excess weight lost over 12 to 54 months.
Risks
Risks common to all surgeries for weight loss include an infection in the incision, a leak from the stomach into the abdominal cavity or where the intestine is connected (resulting in an infection called peritonitis), and a blood clot in the lung (pulmonary embolism). About one-third of all people having surgery for obesity develop gallstones or a nutritional deficiency condition such as anemia or osteoporosis.Fewer than 10 out of 1000 people die after weight-loss surgery.
After a Roux-en-Y gastric bypass:
- An iron and vitamin B12 deficiency occurs more than 30% of the time. About 50% of those with an iron deficiency develop anemia.
- The connection between the stomach and the intestines narrows (stomal stenosis) 5% to 15% of the time, leading to nausea and vomiting after eating.
- Ulcers develop 5% to 15% of the time.
- The staples may pull loose.
- Hernia may develop.
- The bypassed stomach may enlarge, resulting in hiccups and bloating.
What To Think About
Gastric bypass surgery may increase your chances of living longer. Some studies show that people who have weight-loss surgery have a smaller chance of dying of heart problems, diabetes, or cancer.In a gastric bypass, the part of the intestine where many minerals and vitamins are most easily absorbed is bypassed. Because of this, you may have a deficiency in iron, calcium, magnesium, or vitamins. This can lead to long-term problems, such as osteoporosis. To prevent vitamin and mineral deficiencies, you may need to work with a dietitian to plan meals, and you may need to take extra vitamin B12 as pills, shots, or nasal spray.
There is also a possibility that you may develop gallstones after gastric bypass. Sometimes the gallbladder is removed as part of the surgery. But if your gallbladder is not removed, then you may need to take medicine to prevent gallstones.
Early studies of the laparoscopic approach to surgery for obesity suggest that it reduces recovery time and postsurgery complications
Gastric Bypass Surgery
Roux-en-Y gastric bypass surgery uses a combination of restriction and malabsorption to ensure a significant weight loss. During the procedure, the surgeon creates a smaller stomach pouch. The surgeon then divides the small intestine and attaches it to the pouch. The type of connection bypasses a large portion of the small intestine, which absorbes calories and nutrients. Having the smaller stomach pouch causes patients to feel fuller sooner and eat less food; bypassing a portion of the small intestine reduces the amount of calories that can be absorbed by the body.The physicians in the Michael E. DeBakey Department of Surgery perform the gastric bypass laparoscopically. Using this minimally invasive approach, patients heal faster and are able to return to their normal activities more quickly. They also have much less pain, infections, hernias, and overall complications.
Laparoscopic surgery involves making a series of small incisions and inserting long tube-like instruments through them. The abdomen will be filled with gas to help the surgeon view the abdominal cavity. A camera will be inserted through one of the tubes that will display images on a monitor in the operating room. In this manner, your surgeon will be able to work inside your abdomen without making a larger incision.
Specialized instruments are used to laparoscopically perform the Roux-en-Y Gastric Bypass. This is the same gastric bypass as has been performed with the traditional open approach (large incision), but with superior results.
What happens after the surgery?
On the first postoperative day, you will undergo an upper GI to confirm that there are no problems. Following this test, you will begin drinking and be discharged the next day. A follow up appointment will be scheduled in one week and then every several months afterward to ensure that you are enjoying success.What are the risks associated with a Roux-en-Y procedure?
As with any surgery, there are risks such as bleeding, infection, or an adverse reaction to the anesthesia. Other risks include anastomotic leakage, deep venous thrombosis, pulmonary embolism, follow-up operations to correct complications, increased risk for gallstones and nutritional deficiencies such as anemia. Your surgeon will inform you of the risks prior to surgeryWhen can I expect to return to work and/or resume normal activities?
Light activity at home is encouraged after surgery. You can expect to return to normal daily activities, such as showering, and walking up stairs within a few days. If you are taking narcotic medications for pain, you should not drive. Return to work following a laparoscopic gastric bypass is usually between 2-4 weeks.Who is a candidate?
The general criteria used to determine whether you're a candidate are listed below:- BMI >40
- BMI 35-40 with co-morbidities (other medical conditions such as diabetes, heart disease, etc)
- Well-informed, motivated patient
- Previous attempts at medical weight loss programs
- Absence of endocrine orders that cause obesity
What can I expect as a patient?
Step 1: Submit Questionnaire: The first step is to call the Bariatric Coordinator at Baylor College of Medicine's Comprehensive Bariatric Surgery Center and obtain a packet of information and questionnaire. The phone number is 713-798-5662; please ask for Monica Flinn. The questionnaire is a detailed document asking questions about your medical history and previous weight loss attempts. You will need to fill this out completely and accurately and mail it back to the physician's office. Once the physician and his team reviews your questionnaire and considers all the factors involved with your case, they will notifiy if you can proceed to Step 2.Step 2: Obtain referral from your Primary Care Physician (PCP) prior to attending our patient information session. In order to attend the information session we will need you to obtain a clearance letter from your PCP. At this time you should also contact your insurance company to verify that weight loss surgery is covered. If they say that they do NOT cover it, please inquire whether they have any exceptions to that policy. Often if you have certain medical conditions they will cover the surgery.
Step 3: Attend patient information session. The next step is to attend one of our free patient information sessions to assist you in determining whether weight loss surgery is for you. You are encouraged to bring a support person to this session. These sessions include detailed overviews of teh surgery, preparation for surgery and postoperative follow up. You will hear from the surgeon, psychologist, nutritionist, nurse practitioner, financial specialist, and our bariatric coordinator to ensure that all your questions and concerns are addressed. The psychologist will inform you of support groups, emotinal eating classes and other strategies for success. Our nutritionist will explain all the nutritional changes to expect and answer any questions you may have about diet, eating post-surgery, etc. This will be the same nutrionist you meet with for your nutrition consult later in the process. We then have a patient financial services representative take you through the financial process and an insurance specialist to advise you on how to get the surgery covered by your insurance company. Finally, you will meet former patients who have had the surgery and hear their stories and ask them any questions you may have about life after bariatric surgery.
Step 4: Begin preauthorization process with insurance company. There are many types of health insurance policies and many have very strict guidelines for reimbursment. Contact your insurance company for verification of coverage and review your particular policy's guidelines and referral requirements, as well as co-payments. During this step you will work closely with the physician's office to assist you with meeting your insurance company's requirements, including documentation to get your surgery approved by your insurance company. Generally documentation about past weight loss attempts are required. Obtaining this information may require some persistance. Persevere - it will be worth the time and effort.
Step 5: Meet with surgeon and set surgery date. This is fairly straightforward - you meet one-on-one with the surgeon to asses where you are in the process and further discuss the details about the surgery. This is an opportunity for you to delve into the details of your personal case and ask any questions you may still have.
Step 6: Preparation for surgery. Once a surgery date has been decided, our team members will work with you to set up your necessary appointments. Everyone will need to have a chest x-ray, blood work, nutrition consult, and psychological consult. Certain patients will also require a gastroscopy (EGD) or upper GI (UGI). During your meeting with the surgeon, we will also decide if additional medical clearance is necessary from a cardiologist, pulminologist or other medical specialist.
Step 7: Day of Surgery. Prior to surgery we will step you through all detailed pre- and post-surgery instructions. The day of surgery you will come to the hospital early with an empty stomach and let our skilled clinical team prepare and care for you!!
Step 8: Begin the process of healing and feeling better. Successful bariatric surgery begins in the operating room, but it ends in the details of your daily life. It is important to be prepared physically and mentally for the life changes you are about to experience. After surgery, staying hydrated is essential. Careful attention to nutrition and keeping a close relationship with your nutritionist is essential. It is easy to become nutrient deficient if you do not comply with post operative vitamin supplementation. Exercise is another vital component to your success. Simple walks and controlled exercise are important as your body begins to loose weight. Remember our team of exercise specialists are happy to help you create the right exercise plan for you.






0 comments:
Post a Comment