Breast Removal Surgery
In medicine, mastectomy is the medical term for the surgical removal of one or both breasts, partially or completely. Mastectomy is usually done to treat breast cancer; in some cases, women and some men believed to be at high risk of breast cancer have the operation prophylactically, that is, to prevent cancer rather than treat it. It is also the medical procedure carried out to remove breast cancer tissue in males. Alternatively, certain patients can choose to have a wide local excision, also known as a lumpectomy, an operation in which a small volume of breast tissue containing the tumor and some surrounding healthy tissue is removed to conserve the breast. Both mastectomy and lumpectomy are what are referred to as "local therapies" for breast cancer, targeting the area of the tumor, as opposed to systemic therapies such as chemotherapy, hormonal therapy, or immunotherapy.
Traditionally, in the case of breast cancer, the whole breast was removed. Currently the decision to do the mastectomy is based on various factors including breast size, number of lesions, biologic aggressiveness of a breast cancer, the availability of adjuvant radiation, and the willingness of the patient to accept higher rates of tumor recurrences after lumpectomy and radiation. Outcome studies comparing mastectomy to lumpectomy with radiation have suggested that routine radical mastectomy surgeries will not always prevent later distant secondary tumors arising from micro-metastases prior to discovery, diagnosis, and operation.
Side-effects of a mastectomy include:
Complications of mastectomy are uncommon, but can include:
The exact risks are specific to you and will differ for every person, so we have not included statistics here. Ask your surgeon to explain how these risks apply to you.
The technique your surgeon will use will depend on the type of mastectomy you are having.
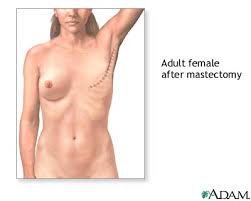
In a simple mastectomy, a diagonal or horizontal cut is made across the breast, and the breast tissue is removed.
Your surgeon may do a sentinel lymph node biopsy and remove lymph nodes from under your armpit through the same cut.
A breast reconstruction may be done at the same time as the mastectomy or at a later date, or not at all.
When the operation is complete, the cuts are closed with stitches (which may be dissolvable).
Fine plastic tubes may be left in your breast area for up to 48 hours afterwards. These allow blood and fluids to drain into a bag.










Traditionally, in the case of breast cancer, the whole breast was removed. Currently the decision to do the mastectomy is based on various factors including breast size, number of lesions, biologic aggressiveness of a breast cancer, the availability of adjuvant radiation, and the willingness of the patient to accept higher rates of tumor recurrences after lumpectomy and radiation. Outcome studies comparing mastectomy to lumpectomy with radiation have suggested that routine radical mastectomy surgeries will not always prevent later distant secondary tumors arising from micro-metastases prior to discovery, diagnosis, and operation.
Rates
Mastectomy rates vary tremendously worldwide, as was documented by the 2004 'Intergroup Exemestane Study', an analysis of surgical techniques used in an international trial of adjuvant treatment among 4,700 women with early breast cancer in 37 countries. The mastectomy rate was highest in central and eastern Europe at 77%. The USA had the second highest rate of mastectomy with 56%, western and northern Europe averaged 46%, southern Europe 42% and Australia and New Zealand 34%.
Mastectomy indications
Despite the increased ability to offer breast-conservation techniques to patients with breast cancer, there exist certain groups who may be better served by traditional mastectomy procedures including:- women who have already had radiation therapy to the affected breast
- women with 2 or more areas of cancer in the same breast that are too far apart to be removed through 1 surgical incision, while keeping the appearance of the breast satisfactory
- women whose initial lumpectomy along with (one or more) re-excisions has not completely removed the cancer
- women with certain serious connective tissue diseases such as scleroderma, which make them especially sensitive to the side effects of radiation therapy
- pregnant women who would require radiation while still pregnant (risking harm to the fetus)
- women with a tumor larger than 5 cm (2 inches) that doesn't shrink very much with neoadjuvant chemotherapy
- women with a cancer that is large relative to her breast size
- Women who have tested positive for a deleterious mutation on the BRCA1 or BRCA2 gene and opt for prophylactic removal of the breasts
- male breast cancer patients
Types of mastectomy
There are a variety of types of mastectomy in use, and the type that a patient decides to undergo (or whether he or she will decide instead to have a lumpectomy) depends on factors such as size, location, and behavior of the tumor (if there is one), whether or not the surgery is prophylactic, and whether or not the patient intends to undergo reconstructive surgery.- Simple mastectomy (or "total mastectomy"): In this procedure, the entire breast tissue is removed, but axillary contents are undisturbed. Sometimes the "sentinel lymph node"--that is, the first axillary lymph node that the metastasizing cancer cells would be expected to drain into—is removed. This surgery is sometimes done bilaterally (on both breasts) on patients who wish to undergo mastectomy as a cancer-preventative measure. Patients who undergo simple mastectomy can usually leave the hospital after a brief stay. Frequently, a drainage tube is inserted during surgery in their chest and attached to a small suction device to remove subcutaneous fluid. These are usually removed several days after surgery as drainage decrease to less than 20-30 ml per day.
- Modified radical mastectomy: The entire breast tissue is removed along with the axillary contents (fatty tissue and lymph nodes). In contrast to a radical mastectomy, the pectoral muscles are spared.
- Radical mastectomy (or "Halsted mastectomy"): First performed in 1882, this procedure involves removing the entire breast, the axillary lymph nodes, and the pectoralis major and minor muscles behind the breast. This procedure is more disfiguring than a modified radical mastectomy and provides no survival benefit for most tumors. This operation is now reserved for tumors involving the pectoralis major muscle or recurrent breast cancer involving the chest wall.
- Skin-sparing mastectomy: In this surgery, the breast tissue is removed through a conservative incision made around the areola (the dark part surrounding the nipple). The increased amount of skin preserved as compared to traditional mastecomy resections serves to facilitate breast reconstruction procedures. Patients with cancers that involve the skin, such as inflammatory cancer, are not candidates for skin-sparing mastectomy.
- Nipple-sparing/subcutaneous mastectomy: Breast tissue is removed, but the nipple-areola complex is preserved. This procedure was historically done only prophylactically or with mastecomy for benign disease over fear of increased cancer development in retained areolar ductal tissue. Recent series suggest that it may be an oncologically sound procedure for tumors not in the subareolar position.
History
Mastectomy for breast cancer was performed at least as early as 548 A.D., when it was proposed by the court physician Aetios of Amida to Theodora. She declined the surgery, and died a few months later.
What are the risks?
Mastectomy is commonly performed and generally safe. However, in order to make an informed decision and give your consent, you need to be aware of the possible side-effects and the risk of complications of this procedure.Side-effects
These are the unwanted, but mostly temporary effects of a successful treatment, for example feeling sick as a result of the general anaesthetic.Side-effects of a mastectomy include:
- soreness, swelling, bruising and tightness in your breast area and in your arm and shoulder
- scarring - you will have a permanent scar, this usually fades over time
- numbness and tingling in your upper arm
Complications
This is when problems occur during or after the operation. Most women aren't affected. The possible complications of any operation include an unexpected reaction to the anaesthetic, excessive bleeding or developing a blood clot, usually in a vein in the leg (deep vein thrombosis, DVT).Complications of mastectomy are uncommon, but can include:
- infection - antibiotics may be needed
- build up of fluid around the healing wound (seroma) - this may require further surgery
- change in sensation in the operated area - this can be permanent
- unusual red or raised scars (keloids) - these can take years to improve
The exact risks are specific to you and will differ for every person, so we have not included statistics here. Ask your surgeon to explain how these risks apply to you.
What happens during mastectomy
Depending on the type of mastectomy you have, your operation may take up to two hours.The technique your surgeon will use will depend on the type of mastectomy you are having.
In a simple mastectomy, a diagonal or horizontal cut is made across the breast, and the breast tissue is removed.
Your surgeon may do a sentinel lymph node biopsy and remove lymph nodes from under your armpit through the same cut.
A breast reconstruction may be done at the same time as the mastectomy or at a later date, or not at all.
When the operation is complete, the cuts are closed with stitches (which may be dissolvable).
Fine plastic tubes may be left in your breast area for up to 48 hours afterwards. These allow blood and fluids to drain into a bag.






0 comments:
Post a Comment